Last Updated on June 16, 2017 by Dr.Derek Fhisher
A new study in the New England Journal of Medicine on treatment of skin infections compares treatment with trimethoprim sulfamethoxazole (TMP-SMX, Bactrim or Septra) or clindamycin. Surprisingly, both worked equally well in this 524 patient study, curing about 89% of outpatients with uncomplicated skin infections cellulitis and abscesses, so the authors appear to encourage use of one of these drugs since they’re better at treating MRSA than are currently recommended antibiotics.
I believe this is a bad idea – it fuels the escalating use of broader spectrum antibiotics with more side effects, at a time when antibiotic development is languishing. It also encourages the “just in case” type of response, rather than prescribers actually thinking about what kind of bacterial infection the patient might have. The authors used a 10-day course of treatment, when expert recommendations are encouraging 57 days treatment to try to reduce risks to patients.
Skin infections are a huge problem. They resulted in 14.2 million outpatient visits in 2005 (the latest year for which statistics are available), and 850,000 hospital admissions, according to the article.
As most cases of uncomplicated cellulitis are caused by Strep, they’re still best treated with a penicillin or cephalosporin (e.g., Keflex) type of antibiotic, known as beta-lactams. These antibiotics are better than TMP-SMX for strep infections. These drugs are safer for widespread use, than clindamycin. Clindamycin and TMP-SMX drugs ought to be reserved for draining or abscesses wounds using a high likelihood of MRSA, not used for every skin infection that is uncomplicated.
While this study adds important information it shouldn’t result in a change in antibiotic treatment recommendations that are current.
The technical details
The study was -done, in that it was randomized and double-blinded, meaning that neither the patient nor the investigator knew which treatment the patient was receiving.
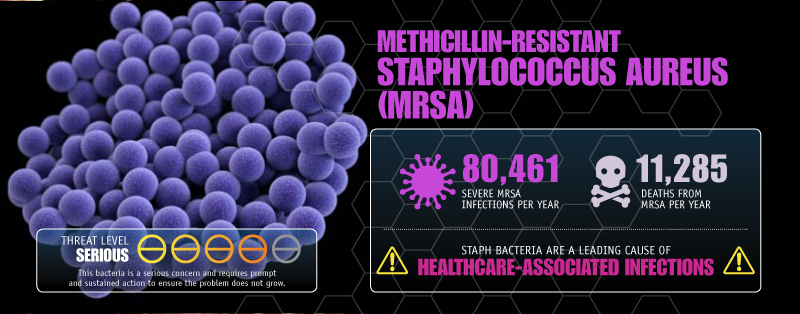
Of note, is that the patients were drawn from areas with a high endemic rate of methicillin-resistant Staph aureus (MRSA) infections. Treatment was with either Clindamycin 300 mg. Three times daily or TMP-SMX, two single strength pills a day, with a fake pill for the third dose. All patients were treated for ten days.
Half of the patients had cellulitis, an infection of the skin and soft tissue. Abscesses occurred in 30.5%, and 16% had both. Cultures may be obtained from S and the abscesses. aureus was isolated in 41.4%; 12% of these isolates were resistant to clindamycin and one was TMP-SMX resistant.
While not stated explicitly, the authors imply that either clindamycin or TMP-SMX are the best choices for uncomplicated cellulitis, as this worked and covers MRSA.
Based on my 30 years of experience as an infectious diseases practitioner and literature, I ‘ve several concerns regarding this shift in treatment and focus .
First, nonpurulent cellulitis, meaning one where there isn’t any abscess or drainage to culture), is most commonly caused by Streptococci, not Staph. Recommendations from both the Infectious Diseases Society of America (IDSA) and UpToDate are to use a beta-lactam type drug, I.e., a penicillin or cephalosporin. Typical choices would be dicloxacillin, or penicillin, or cephalexin, which adds coverage for “regular”or methicillin-susceptible Staph, though some use clindamycin. TMP-SMX wasn’t used for strep infections; if uncertain about whether an infection was due to Staph or Strep, some used TMP-SMX in combination with amoxicillin.
Another cellulitis study found that 73% of hospitalized patients had beta-hemolytic streptococci as the causative agent; this had a 97% response using a beta-lactam.
One recognizable type of cellulitis is erysipelas. This is distinctive, with a sharply demarcated border and skin that’s thickened (indurated) and often bright red. This really is treated with penicillin and is caused by Strep. It doesn’t respond to TMP-SMX or vancomycin. I’m concerned that a trend towards treating everything by algorithm or “what if it may be MRSA?” will result in more mistreatment of the common skin infection. With fewer physicians I wonder just how many people will recognize this in the future.
Another randomized, double-blind trial compared cephalexin to that plus TMP-SMX for treating uncomplicated cellulitis.? There clearly was no benefit to the addition of coverage for MRSA, supporting the recommendation that is traditional to use a beta- lactam.
By comparison, with purulent (pus) cellulitis, MRSA becomes a larger concern, and empiric treatments with clindamycin, TMP-SMX, or doxycycline are generally used.
Inside my experience, which is more with hospitalized patients many patients who receive TMP-SMX or Vancomycin for cellulitis fail therapy. Beta-lactams (penicillin or cefazolin) are the drug class of choice for cellulitis. Clindamyin is used for septic patients for its anti-toxin effect.
There are other problems I see together with the approach of using these two antibiotics “just in case” it’s MRSA, even when the probability is that it won’t be. While there might not be good studies common experience is that higher doses of TMP-SMX are needed for MRSA. Certainly, I’ve noticed a need for higher doses in my obese patients and even in the young, muscular, football player types.
I prefer Keflex types or penicillins of antibiotics empirically for two other reasons. One is that there appear to be fewer serious side effects than. difficile infectious diarrhea, or TMP-SMX. The latter causes the worst drug rashes I’ve ever seen. It can also cause anemia, either by bone marrow suppression, or by hemolysis in African-Americans, Asians, and Latinos, due to a glucose-6 phosphate dehydrogenase (G6PD) deficiency. In the U.S., G6PD deficiency has a 10% prevalence in black men. One small study found no problem with patients receiving TMP-SMX?. Severe hemolytic anemia was found by another series? in HIV patients receiving TMP-SMX concluding, as did a study in army personnel?, that screening of at-risk populations is warranted, especially should they’ve HIV? Well.
Another concern is whether resistance will be promoted by widespread use of clindamycin at a time when we’ve limited options that are antibiotic.
Current recommendations are to treat abscesses that are small with no antibiotics and drainage and incision. An abstract at the IDWeek conference suggests that treatment with TMP-SMX as well provides additional benefit.
The final disconcerting note in this report is that the authors used a 10 day course of therapy. The trend is to try to limit antibiotic exposure for serious infections like pneumonia. For longer for cellulitis, the IDSA guidelines?recommend 5 days treatment; many physicians but few treat. Dr. Loren Miller, the study’s lead author, told me that pediatricians insisted on the 10 day course. I’d hope that such an opinion poll WOn’t be the sole driver of a change in practice.
I agree with all the accompanying editorial that non-purulent cellulitis is treated with a beta-lactam. There isn’t any demonstrated need for using TMP-SMX or clindamycin for uncomplicated cellulitis, and they need to be reserved for draining or abscesses wounds with culture proven infection, or a high likelihood of MRSA. The authors saw a 12% rate of resistance to clindamycin. Increased non-essential use is likely to push that higher.
The new study adds important “and surprising news” that either of these drugs works well for uncomplicated skin infections. It shouldn’t be a game changer over current recommendations.



No Comments Yet